oxygen levels in children chart
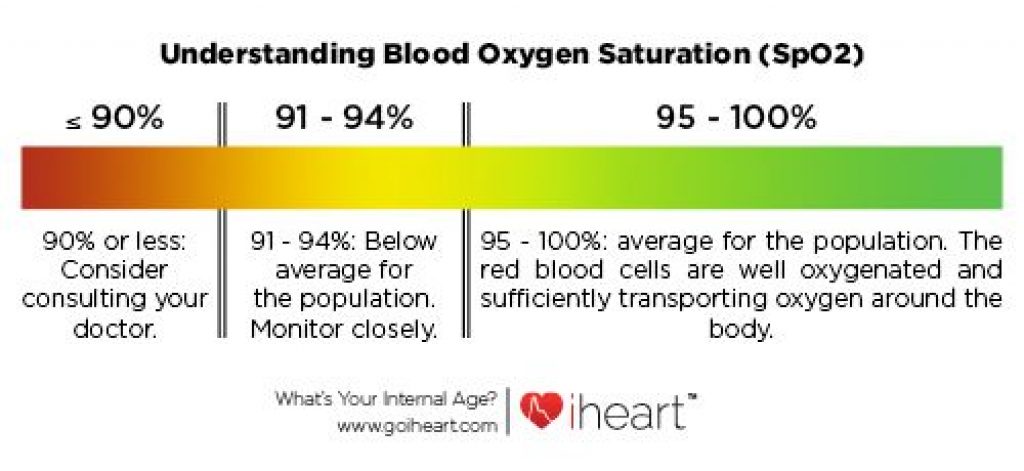
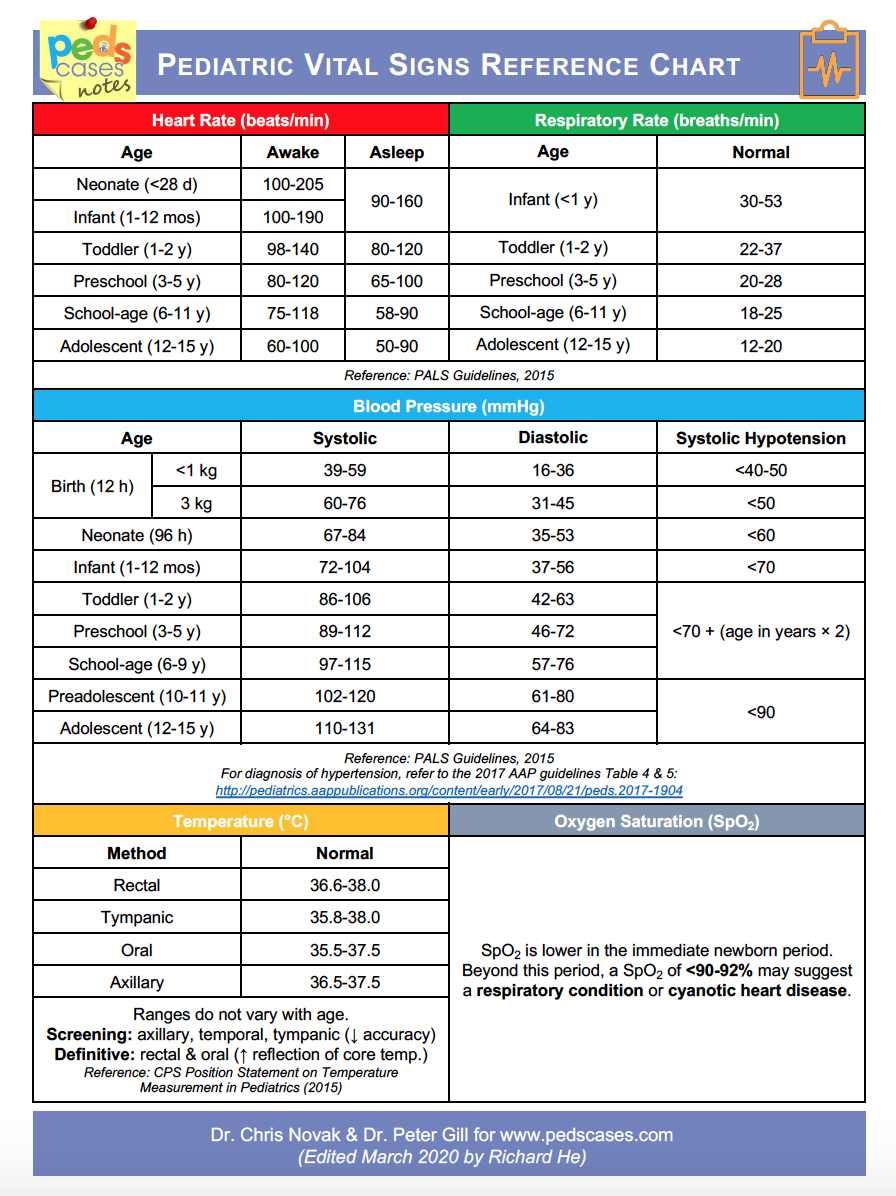 Pediatric Vital Signs Reference Chart | PedsCases
Pediatric Vital Signs Reference Chart | PedsCasesYour account has been temporarily blocked due to the wrong signal in the attempts and will automatically unlock 30 minutes. For immediate assistance, contact the Customer Service: 800-638-3030 (United States), 301-223-2300 (international) Log inLippincott Magazine Subscribers, use your username or email along with your password to log in. Registration of a free account Registered users can save items, searches and manage email alerts. All registration fields are necessary. Side Logos Colleague's email is Invalid Your message has been sent to your colleague. Final note Procite Reference Manager Save my selection Can a pulse oxygen saturation from 95% to 96% help predict greater destabilization of vital signs in school-age children? A retrospective observational study Kobayashi, Masaru MD*; Fukuda, Shinya MD; Takano, Ken-ichi MD, PhD; Kamizono, Junji MD; Ichikawa, Kotaro MDEditor(s): Moawad, Eman Mohamed I.Pediatric Emergency assistance, Kitakyuhatshu Municipal Hospital Yahata, Kitakyushu, Fukuoka Abbreviations: 95% CI = 95% confidence interval, CTAS = Triage and Acuity Scale of the Canadian Emergency Department, HR = heart rate, IQR = interquartile range, PEWS = Pediatric Early Warning System, RR = respiratory rate. The authors declare that there is no conflict of interest. This is an open access article distributed under the terms of the Creative Commons Attribution-Non 4.0 Commercial License (CCBY-NC), where it is possible to download, share, remix, transform and build the work that is correctly cited. The work cannot be used commercially without permission from the journal. Received December 7, 2017Accepted May 24, 2018 Summary To determine whether a peripheral oxygen capillary saturation (SpO2) of 95% to 96% should be considered "non-emergency" in school-age children, as suggested by the Canadian Emergency Department Triage and Aquatic Scale. Children of school age (6-12 years) with a normal body temperature (36.5–37.4°C) who visited our department between September, 2014 and August 2015 (n = 4556) were divided into 4 groups based on SpO2: group A: 99% to 100%; group B: 97% to 98%; group C 95% to 96%; and group D: ≤94%. The heart rate (HR), the respiratory rate (RR) and the hospitalization rate were compared between the groups, and also among children with SpO2 95% to 96% and the controls combined with SpO2 ≥97% (n = 280 each). Among 4556 eligible patients, groups A, B, C and D included 2700 patients (59.3 per cent), 1534 patients (33.6 per cent), 280 patients (6.2 per cent) and 42 patients (0.9 per cent), respectively. The median (interquartile range [IQR]) RR increased significantly with the decrease in SpO2 (23 [20-25], 24 [20-26], 24 [23-30], and 30 [24-40] breaths/min in A-D groups, respectively; P An SpO2 95% to 96% among school-aged children should not be considered "non-emergency", but a significant clinical situation requiring early review of RR and RR. Rapid interventions among this group of children will help prevent new destabilizations of vital signs, which in turn will contribute to reducing health care costs.1 IntroductionThe peripheral capillary oxygen saturation (SpO2) is widely used to evaluate the urgency during pediatric care, and is usually included in the vital evaluation of the child's sign. The SpO2 criterion is included in some triage systems, including the triage and acute system of the Canadian Emergency Department (CTAS), the emergency gravity index, the Australian triage scale and the Manchester triage system. The 5-level pediatric CTAS triage system (level I, resuscitate; level II, emerging; level III, urgent; level IV, less emerging; and level V, non-emergency) is based on complaints and medical conditions for children and has been used in the pediatric emergency environment of the major Japanese health-care institutes for more than 10 years. Although a SpO2 2 Methods This population-based retrospective study was conducted at the Pediatric Emergency Center at Kitakyushu Yahata Municipal Hospital, Japan, using data from September 2014 to August 2015. The hospital is a tertiary reference centre for the community pediatric department and is 19 m above sea level. The reporting guidelines for STROBE were used in the design and implementation of our research. Patient data were collected from electronic medical lists. In the case of the population surveyed, school-age children who are consulted at the general hospital for intrinsic or extrinsic reasons were targeted. Of patients who were subjected to triage by the pediatric early warning system (PEWS) in our hospital during the study period, we included children of school age (6-12 years) with a normal body temperature (36.5–37.4°C). Children were divided into 4 groups based on their SpO2 level: group A—99% to 100%; group B—97% to 98%; group C—95% to 96%; and group D—≤94%. The primary results were differences in heart rate (HR), respiratory rate (RR) and hospitalization rate among groups. The HR, RR and SpO2 were measured concomitantly. The Kruskal-Wallis test was used to compare the average values of continuous variables (such as age) and the proportions of categorical variables between groups. Data for non-parametric continuous variables were expressed as the median ± interquartile range (IQR). In addition, differences in hospitalization rates were calculated using the qui-table test. For the comparison between children with a SpO2 of 95% to 96% and an age control group and children with sex partners with a SpO2 ≥97%, the control group was selected from 4234 cases of SpO2 ≥97%. As a total of 280 patients had a SpO2 of 95% to 96%, a cohort of 280 patients was selected as a control group. To compare these 2 groups, the Mann-Whitney U test was used for all tests except for the hospitalization rate, which was calculated using the chi-square test. The results were analyzed using PRISM software (version 7; GraphPad, San Diego, CA). The significance threshold was the approval of P Study of the Institutional Review Board of the Pediatric Emergency Center of the Kitakyushu Municipal Hospital. Since the study data were anonymous, the requirement for informed consent was waived.3 Results Of the total of 41,512 patients who were subjected to triage during the study period, children who were ≤5 years or ≥13 years were excluded (n= 31.814), along with those who had errors in their medical records with respect to SpO2 (n = 12). After applying the exclusion criteria, 4556 children aged 6 to 12 years were included with a normal body temperature (). Of these, 2700 (59.3%), 1534 (33.6%), 280 (6.2%) and 42 (0.9%) patients were classified as groups A (SpO2, 99% – 100%), B (SpO2, 97% – 98%), C (SpO2, 95% – 96%), and D (SpO2, ≤ 94%), respectively. Medium RR (IQR) increased significantly as SpO2 decreased: group A, 23/min (20–25/min); group B, 24/min (20–26/min); group C, 24/min (23–30/min); and group D, 30/min (24–40/min) (P ≤ 0.01) (A). Similarly, the median (IQR) HR increased significantly as the SpO2 decreased: group A, 93 per minute (bpm) (83–104 bpm); group B, 98 bpm (87–110 bpm); group C, 107 bpm (93–119 bpm); and group D, 121 bpm (109–137 bpm) (P RR and RR cases were significantly different. This showed that HR was significantly different, at 105 bpm compared to 97 bpm (P 4 Discussion) In the present study, the RR, HRR and hospitalization rate was significantly higher in school-age children with a SpO2 of 95% to 96% compared to those with a SpO2 of 97% to 100%. In addition, the observed increase in heart rate between 95% and 96% of the saturation group made the PEWS score increase by 2 points, and in patients with a ≤94% saturation, the PEWS score rose by 3 or more points. In addition, in considering the increase in HRR from 95% to 96% of the group, the patient's presentation was at level 3 or 4 instead of level 5 according to TCAS. Although the hospitalization rate of group C (SpO2, 95%–96%) was only 10%, this hospitalization rate was 2.2 times higher than that of group B (SpO2, 97%–98%), and 2.8 times higher than that of group A (SpO2, 99%–100%). In addition, the hospitalization rate in group D (SpO2, ≤94%) was approximately 40%, which was 4 times higher than that of group C. Together, these findings suggest that the patient's oxygen saturation can help predict the severity of a condition, and also underline the need for closer observation of the patient. Therefore, if a patient does not live at a high altitude, a SpO2 should not be discarded from 95% to 96% as a "non-optimal" in the establishment of pediatric emergencies. It should be noted that in this study, although there was a statistically significant difference in RR, there was no clinically significant difference in RR between groups with SpO2 95% to 96% and 97% to 100%. Instead, HRR in the group with SpO2 95% to 96% was significantly higher than in the group with SpO2 97% to 100%, both statistically and clinically. A recent study of retrospective cohorts reported that oxygen saturation from 95% to 96% is suitable for children admitted to the hospital; however, it was reported that these values are associated with respiratory infection of respiratory, lung or cardiovascular systems. The same was also considered from the proportion of diseases hospitalized in 95% to 96% of the group in this study. Previous reports have suggested that a SpO2 ≤95% is abnormal and requires intervention, especially in patients with pneumonia or asthma. In addition, a study suggested that a SpO2 ≥97% is common in healthy school-age children. Despite these reports, no global standard value has been established for SpO2 in children. The normal SpO2 values have been reported recently in several populations. An SpO2 ≥97% was reportedly normal in a study performed in Hawaii, whereas an SpO2 of 98.5% was considered the reference value for children aged 1 month to 5 years in India. In Papua New Guinea, median SpO2 was 98 per cent (IC95% 97.5 per cent–98.0%) for children aged 5 years. In the United States, the average SpO2 was 98.7 per cent (IC95% 98.6 per cent–99.8 per cent) for children aged 5 to 15 years. Therefore, a SpO2 of 95% to 96% in school-age children living at sea level should not be discarded as a "non-emergency" presentation, but understood as a condition that has clinical significance for the pediatric emergency care environment. Some reports have been documented showing a decrease in the average oxygen saturation and higher altitude HRH. For this reason, the conclusions of this study are relevant only at the sea level. The present study has some limitations. First, this was a retrospective study carried out in a single center. Therefore, the selection bias may be present. Furthermore, because our hospital is an emergency hospital, treatment and hospital bias may also exist. Second, it is difficult to assess the vital signs in children due to their tendency to get emotional and restless, both of which can result in fluctuations in RRH and RR. Therefore, standardized measurement methods are needed, and also future prospective studies to record and analyze the response and time to respond by saturation level. Finally, we do not study saturation relationships and specific types of diseases or compare these with RR and RR changes. Therefore, future studies are justified to evaluate these potential relationships. This is the first known study of the relationship between oxygen saturation levels and adverse events in pediatric emergency patients with normal body temperature at sea level. We showed that the rate of RR, HRR and hospitalization was significantly higher in school-age children with a SpO2 of 95% to 96% compared to those with a SpO2 of 97% to 100%. These results suggest that a SpO2 of 95% to 96% should not be discarded as not urgent. Instead, a careful review of HRH and RR should be undertaken to facilitate timely assessments and interventions, thereby reducing related health care costs. Moreover, by understanding the first signs of the vital destabilization of signs among school-age children, the quality of triage decision-making could be improved. Recognition We would like to thank Editage for help in the language edition of the manuscript. Author's contributions MK and SF conceived the study and its design; MK, SF, KT and JK collected the data; SF, KT, JK and KI managed, analyzed and interpreted the data. All authors have read and approved the final manuscript. This manuscript has not been published or presented elsewhere or in its entirety and is not considered by another journal. Conceptualization: Masaru Kobayashi, Junji Kamizono. Data Commissioner: Masaru Kobayashi, Shinya Fukuda, Ken-Ichi Takano, Junji Kamizono. Formal analysis: Masaru Kobayashi, Shinya Fukuda, Ken-Ichi Takano, Junji Kamizono. Research: Masaru Kobayashi, Shinya Fukuda, Ken-Ichi Takano, Junji Kamizono. Methodology: Ken-Ichi Takano, Junji Kamizono. Project Management: Masaru Kobayashi, Shinya Fukuda, Ken-Ichi Takano, Junji Kamizono, Kotaro Ichikawa. Resources: Masaru Kobayashi. Software: Ken-Ichi Takano. Validation: Masaru Kobayashi, Ken-Ichi Takano, Junji Kamizono, Kotaro Ichikawa. Write – original draft: Masaru Kobayashi. Drafting – review " edition: Masaru Kobayashi, Ken-Ichi Takano, Junji Kamizono, Kotaro Ichikawa.ReferencesCanadian Scale of Triage and Acuity; heart rate; respiratory rate; school-age population; SpO2 Source Colleague's email is Invalid Your message has been sent to your colleague. Thank you for registering! Be sure to check your new user account in the next 24 hours", "Related ArticlesFollow Medicine® in Social Media! Colleague's email is Invalid Your message has been sent to your colleague. Final note Procite Reference Manager Save my selection Article level metrics Keywords Keywords Featured Note the keywords selected in the text of the article. Canadian Triage and Acuity Scale heart rate Respiratory rate school-aged population SpO2 Search for similar items You can search for similar items that contain these same keywords or can modify the list of keywords to increase your search. Related links Related videos Readers of this article Read also Never miss a numberBrowse Journal ContentFor Journal Authors Customer Service This website uses cookies. By continuing to use this website, you are consenting to the cookies used. For information about cookies and how you can disable them, visit our policy and ours.

Pin on blood oxigen
EARLY WARNING SCORES All adult patients cared for in all UK hospitals will have their observations monitored using the NEWS Track and Trigger Score. This is described in the RRAPID e-book. In children there is no single standardised Early Warning ...
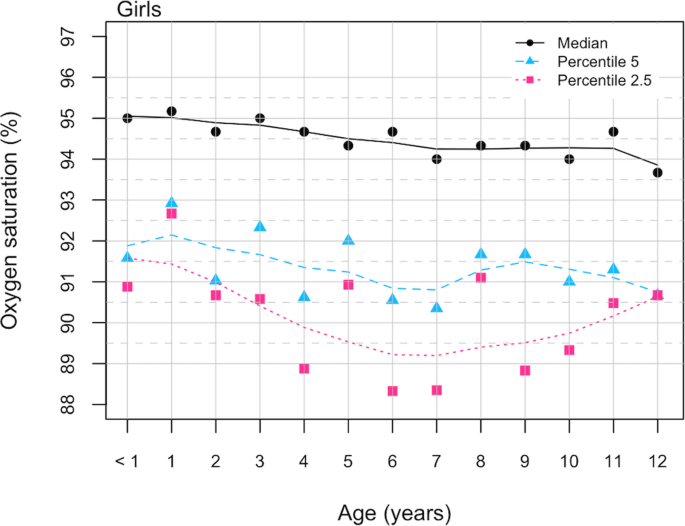
Pulse oximetry curves in healthy children living at moderate altitude: a cross-sectional study from the Ecuadorian Andes | BMC Pediatrics | Full Text

PDF) Reference values for oxygen saturation by pulse oximetry in healthy children at sea level in Chennai

Blood Oxygen Level Chart - Gallery Of Chart 2019
What is an oxygen level chart? - mccnsulting.web.fc2.com

Ill and Feverish Child. Medical information. Causes of fever | Patient
Clinical Guidelines (Nursing) : Observation and continuous monitoring
Congenital Heart Defects Information for Healthcare Providers | CDC

What is an oxygen level chart? - mccnsulting.web.fc2.com

Oxygen Saturation Targets in Preterm Infants and Outcomes at 18–24 Months: A Systematic Review | American Academy of Pediatrics
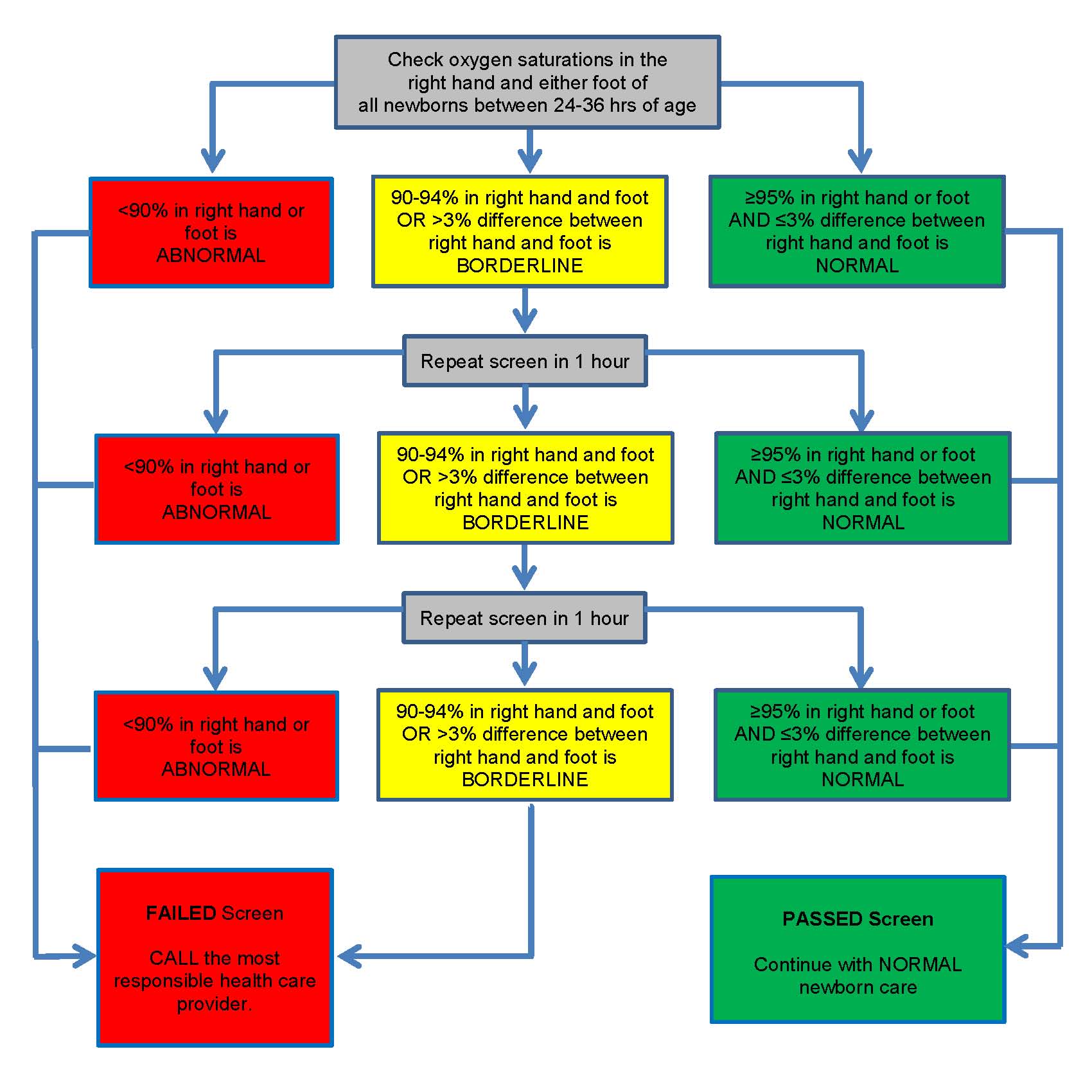
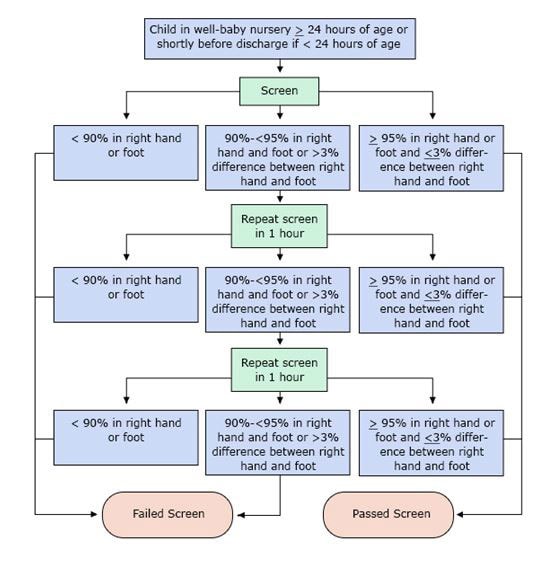
Pulse oximetry screening in newborns to enhance detection of critical congenital heart disease | Canadian Paediatric Society

PDF) OXYGEN SATURATION TRENDS IN NEWBORN AFTER BIRTH
7 Best Pulse Oximeter for COPD, Cardiovascular disease, Sleep apnea
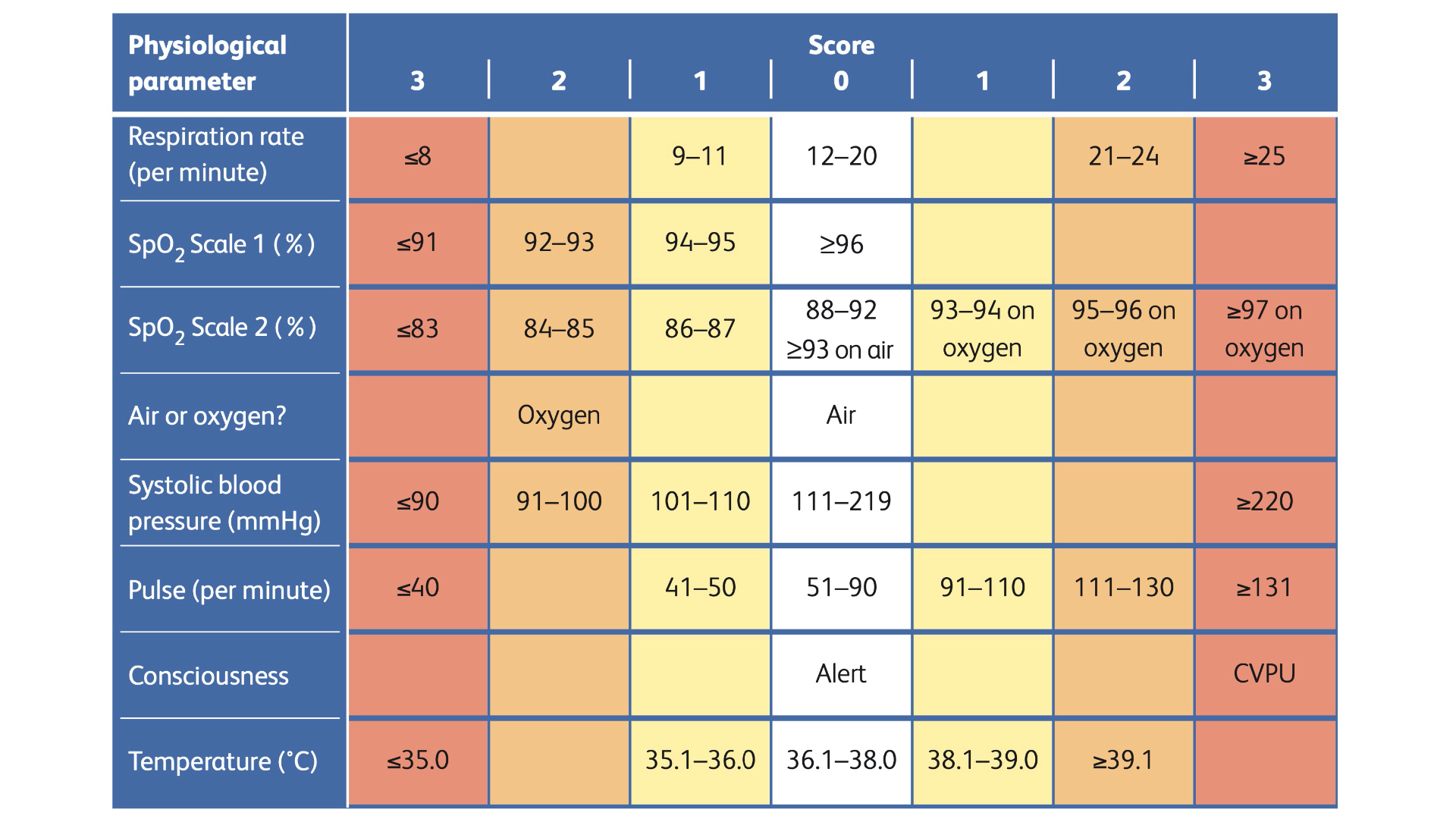
Measuring Basic Observations (Vital Signs) - OSCE Guide | NEWS2 | Geeky Medics

Pediatric Vital Signs Reference Chart | Pediatric vital signs, Pediatric nursing, Pediatrics
Clinical assessment tool for children 0-5 years Traffic light system for identifying severity of illness
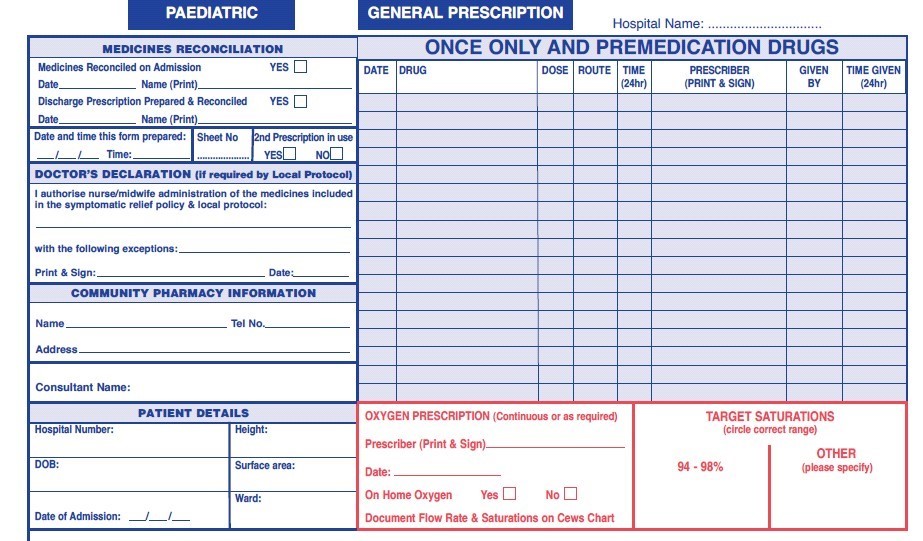
Oxygen: prescription and administration in children
Clinical Guidelines (Nursing) : Oxygen delivery
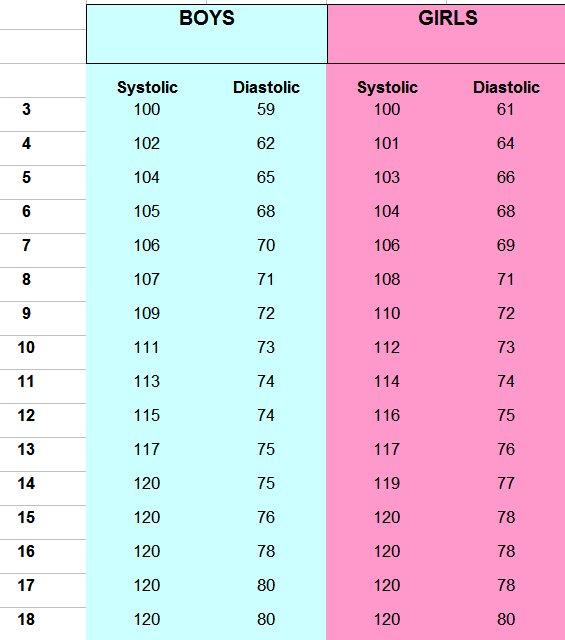
Blood Pressure Chart

PDF) Defining the Reference Range for Oxygen Saturation for Infants After Birth

The utility of high-flow nasal oxygen for severe COVID-19 pneumonia in a resource-constrained setting: A multi-centre prospective observational study - EClinicalMedicine
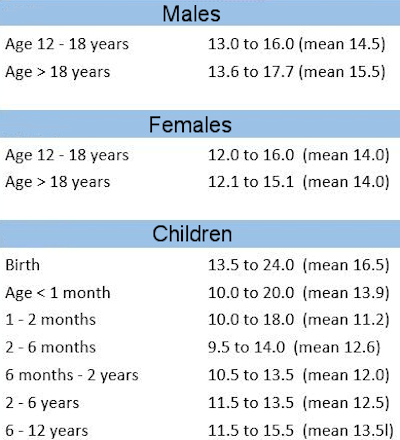
Hemoglobin Level Chart - Body Iron Information | Disabled World
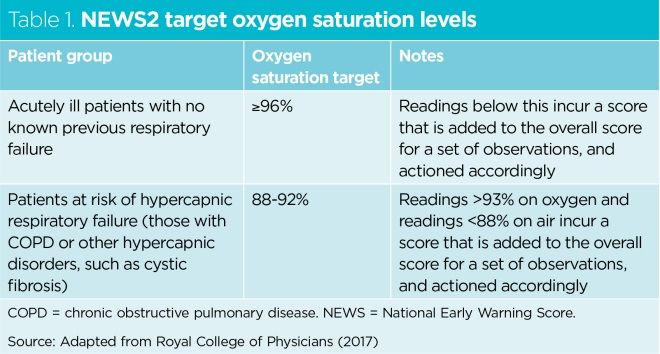
Ensuring the safe use of emergency oxygen therapy in acutely ill patients | Nursing Times
What is an oxygen level chart? - mccnsulting.web.fc2.com

Acute Asthma and Other Recurrent Wheezing Disorders in Children - Clinical Evidence Handbook - American Family Physician
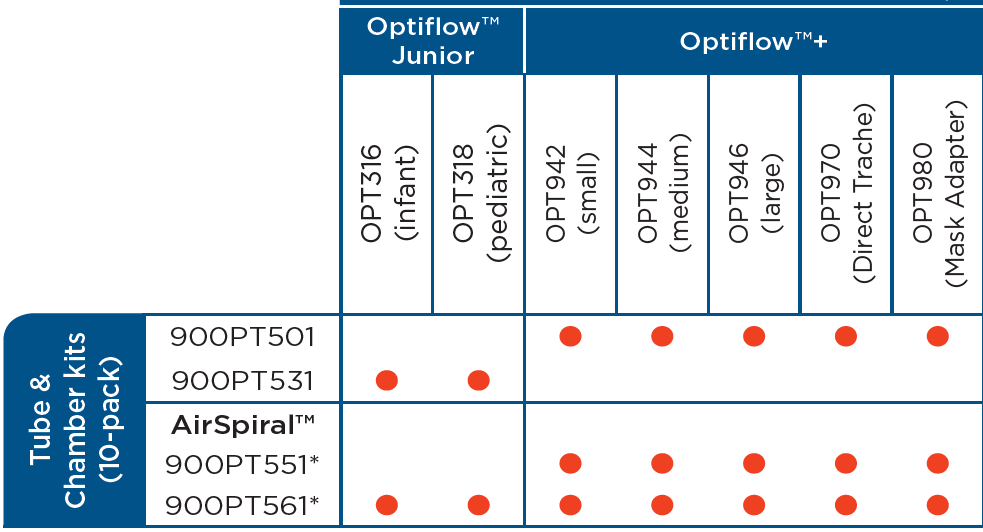
Clinical Guidelines (Nursing) : Oxygen delivery

Coronavirus: MOH spells out proper use of oxygen level tracking device, Health News & Top Stories - The Straits Times
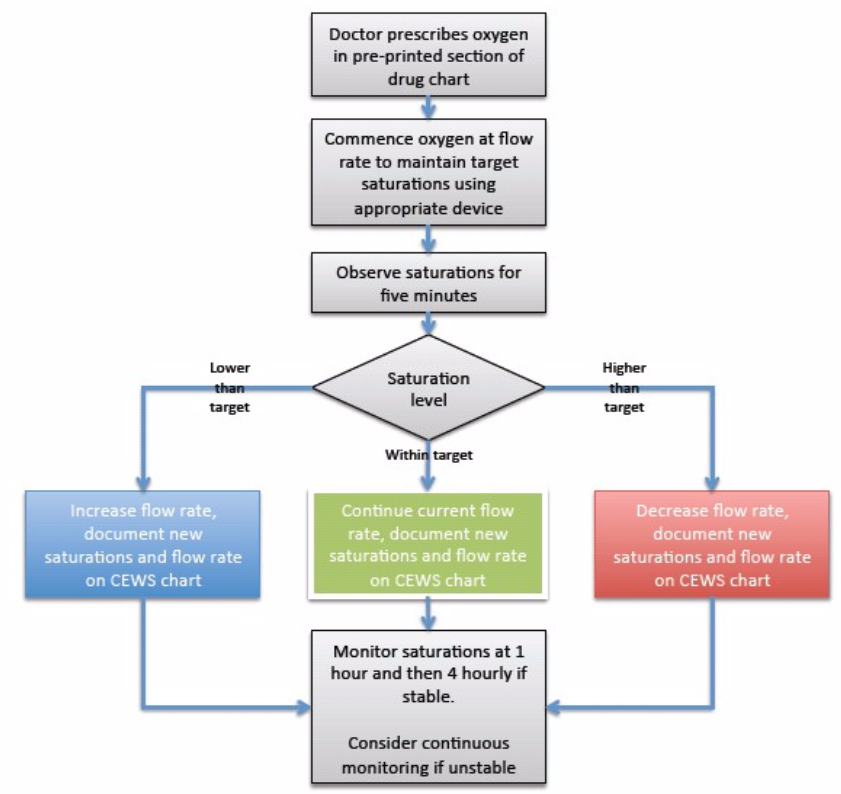
Oxygen: prescription and administration in children

Effects of high altitude on respiratory rate and oxygen saturation reference values in healthy infants and children younger than 2 years in four countries: a cross-sectional study - The Lancet Global Health

Blood Oxygen Level Chart - Gallery Of Chart 2019
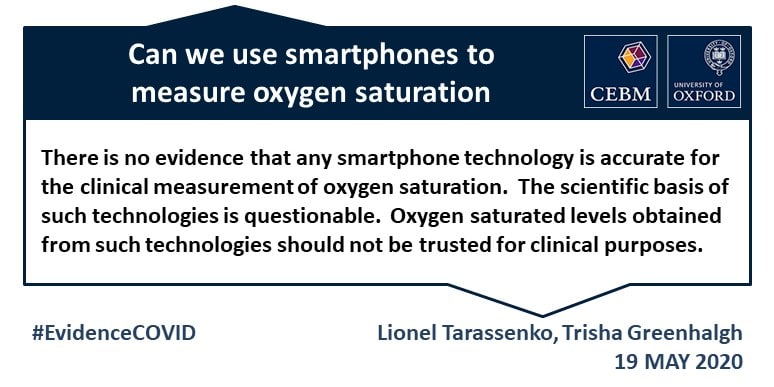
Question: Should smartphone apps be used clinically as oximeters? Answer: No. - The Centre for Evidence-Based Medicine
Bradycardia and Apnea in Premature Babies
EARLY IDENTIFICATION AND MANAGEMENT OF SEVERE SEPSIS AND SEPTIC SHOCK IN CHILDREN AND YOUNG PEOPLE

BTS guideline for emergency oxygen use in adult patients | Thorax

Pulse oximetry in primary care | GPonline

Wireless, implantable catheter-type oximeter designed for cardiac oxygen saturation | Science Advances

Pulse Oximetry and the Neonate | American Academy of Pediatrics
Pulse Oximetry Training Manual
How a Popular Medical Device Encodes Racial Bias | Boston Review
Posting Komentar untuk "oxygen levels in children chart"