 Adverse reactions to local anesthetics | Registered Dental Hygienist (RDH) Magazine
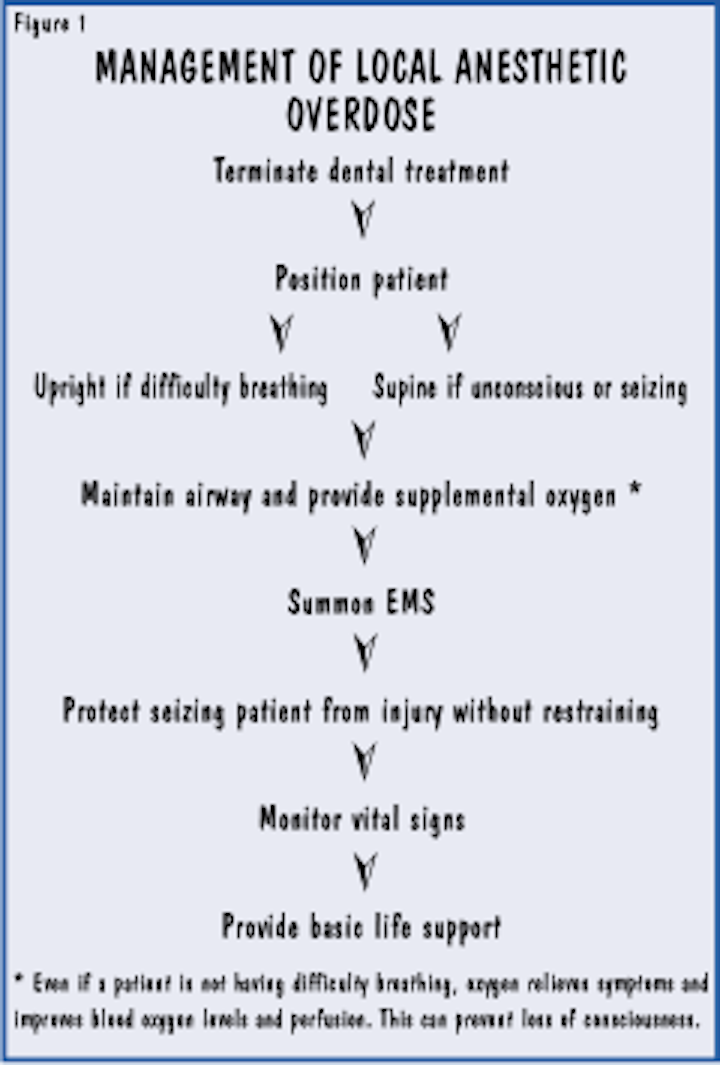
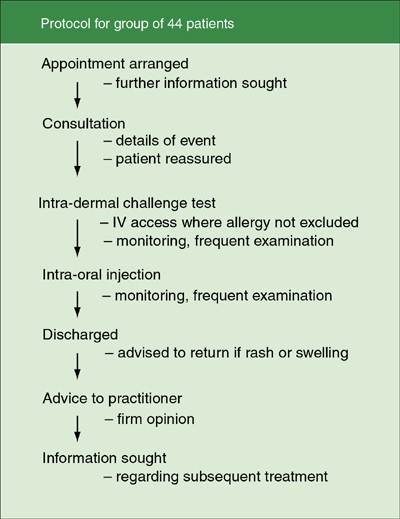
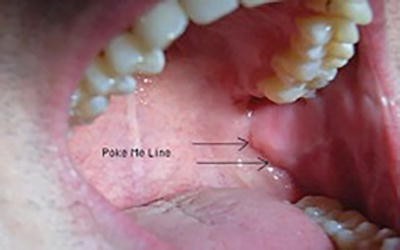
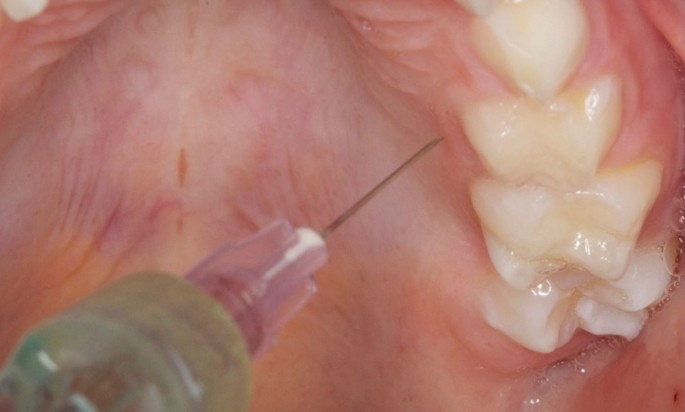
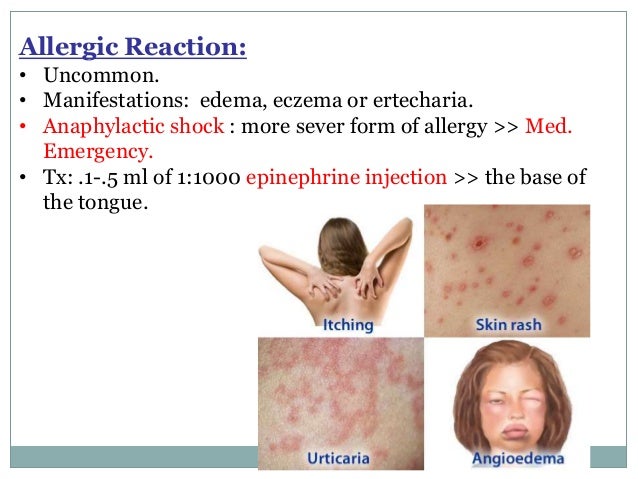
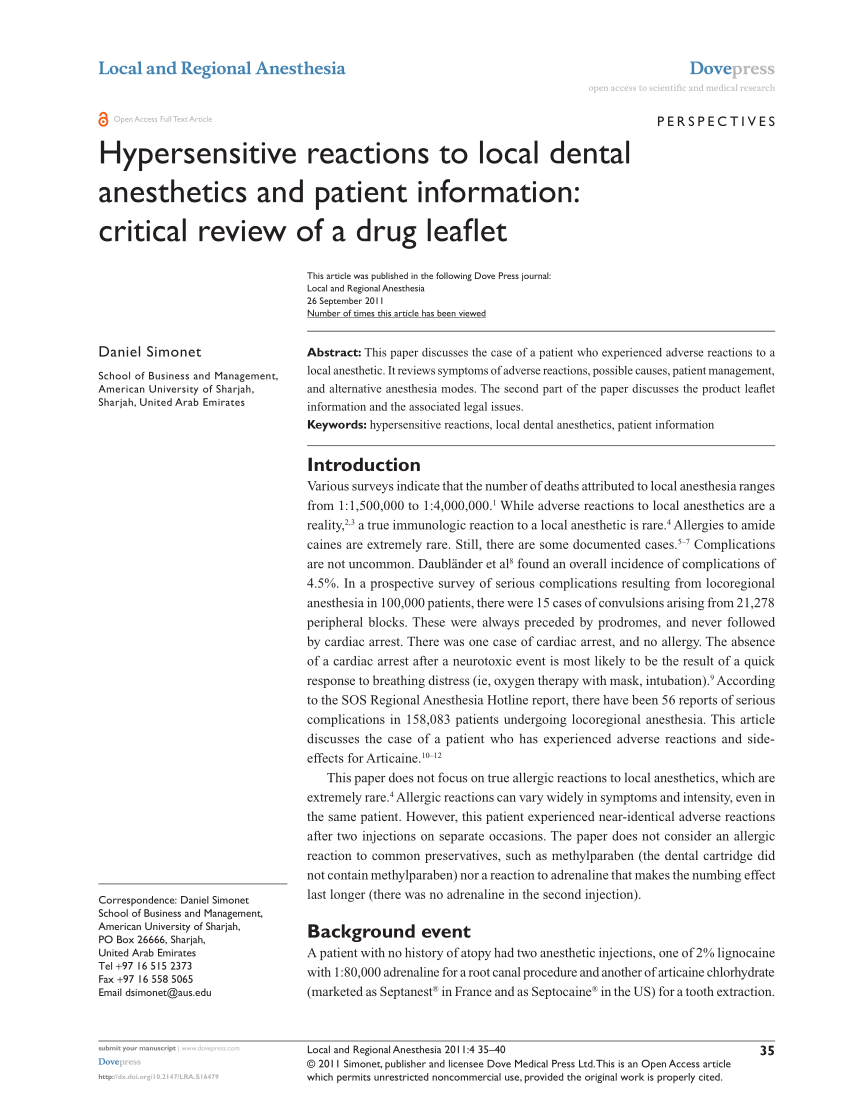
Adverse reactions to local anesthetics | Registered Dental Hygienist (RDH) MagazineThanks for visiting nature.com. You are using a browser version with limited support for CSS. To get best experience, we recommend you to use a more up-to-date browser (or turn off the compatibility mode in Internet Explorer). In the meantime, to ensure continuous support, we are showing the site without styles and JavaScript.WarningAnesthesiaAn adverse reaction to injection local anaesthesia dental — 'allergy' is not the cause volume 189, pages380-384(2000) volume 1897243 Accesses1 AltmetricAbstractObjective Investigate patients considered to have experienced allergic reactions to local anesthesia administered for dental treatment. ObjectiveSetting Dental facility within a general hospital. AdjustmentProcedures Intraoral and skin challenge tests. ProceduresResults No allergic patient was found to lignocaine or prilocaine. The most likely causes of adverse reactions were found as psychogenic. ResultsConclusion Although the allergy to ignocaine (and other agents amide anesthesias used in dentistry) is very rare, it is still suggested as a cause when adverse reactions to dental injections occur. Psychogenic reactions are the main causes of undecided events, and some may be alarming. A lower proportion of adverse responses to intravascular (evitable) injections can be attributed. Adverse reactions can be reduced if injections are administered carefully. Conclusion Main The careful management of the local anesthesia solution to facilitate dental treatment is an extremely safe procedure. However, temporary and trivial adverse reactions are common, but some give rise to concern. Allergy responses to the local anaesthesia of the amidea used in dentistry are extremely rare., Many series of patients have been reported researched by 'suspectful allergy', but in most cases hypersensitivity to local anesthetic agents was excluded. Exceptional cases have been reported in which an allergic response has been confirmed to one of the anesthesias commonly used in dentistry (e.g. lignocaine, mepivacaine prilocaineor) or another component of the dental product (e.g. methylparaben, metabisulfite). This report summarizes the research of patients referred by dental colleagues for "allergy tests" and the results reinforce the nature of adverse reactions that are commonly found. MethodThe first group of 97 patients was investigated for a period of 5 years (1976-1981). The history of the adverse event was documented and patients reported that the test procedure was designed to identify whether they had experienced an allergic reaction to the local anesthetic agent used. The investigations were carried out in a recovery area in a general anesthesia suite, with complete resuscitation facilities and nursing supervision. Intra-dermal injections of plain lignocaine and normal saline (control) were performed in the first 31 patients, then the test procedure included smooth prilocaine in the later 66. Between 1982 and 1994, many patients were seen with similar problems, but the details of their management were not retained. During this period, feedback from practitioners revealed that the negative results of skin tests alone did not convince the patient or practitioner that the medications were safe to use in dentistry. Accordingly, the test procedure was amended. The following protocol () was adopted for the smallest group of 44 adult patients, investigated for 3 years (1994–96). This protocol is similar to the recently reported, but performed in a dental environment. Graph 1Dragm Reference Protocol Preliminary arrangements Upon receiving the referral, a half-week appointment was arranged and the patient was informed that the visit would involve at least 3 hours in the hospital. Where possible, additional information was requested on the negative fact of the practitioner concerned. Preparation In consultation, a complete story was obtained, to specifically include: The nature of the adverse event (this often proved the most informative aspect of history). Prior dental care, including the use of local anesthesia. Personal history of any event or disorder that may indicate a topical background; associated family history. The origin of the suggestion that the patient may be allergic to local anesthesia. The trial process was explained and consent was obtained. It was generally possible to inform the patient at this stage that, from history alone, a true allergy could be excluded, so that the test procedure would be comfortable and provide useful information to help their future management. A firm and safe approach was adopted to reassure the patient. The test procedure was organized in dental surgery and adjacent recovery area within a general hospital, which were equipped with emergency medications and equipment. The procedures were carried out with the help of a trained nurse who monitored the patient during observation periods. The test procedure The patient was sitting in the dental chair, which was then tilted for the patient to be semi-reconnected. Baseline recordings of the patient's pulse rate, blood pressure and oxygen saturation were obtained. Pulse oxide remained in position during the tests. In cases where history could not exclude an allergic reaction, venous access was guaranteed. Intra-dermal direct challenge tests were performed on the skin of the forearm flexor surface (which was cleaned using sterile saline). The test consisted of intra-dermal injections of 0.1 ml of 0.5% lignocaine and 0.5% prilocaine (both vasoconstrictor and no preservative plain), and normal saline (as control). Although skin tests have been criticized (such as positive and negative false reactions occur), they remain valuable as part of the test procedure. The injection site and the overall condition of the patient were closely observed during the first 15 minutes, and then at intervals of 15 minutes up to 1 hour. In the absence of an immediate response, the second stage of the procedure was carried out. A "dental" challenge test was performed. The dental chair was placed to make the patient completely reclined. 1.0 ml of 2% lignocaine with adrenaline (Xylocaine, Astra) was administered as a maxillary oral infiltration adjacent to the second premolar. The patient was monitored for one more hour, including the re-examination of skin testing sites. At the end of the observation period, the patient was discharged, but was asked to contact or return to the hospital the following day (or later) if they had any concerns and, in particular, if they had any inflammation, itching or rash. Follow-up When the test procedure was completed, a letter was sent to the dental doctor (with a copy to any colleague involved with the referral) with a firm recommendation on patient management. A few months later, another letter was sent to the dental doctor, asking about the patient's later address. ResultsFirst group ()Figure 2Results from the first group Of the initial series of 97 patients undergoing intra-dermal defiance tests, none were allergic to anesthetic agents, which always included ignocaine, and for most patients they also involved prilocaine (no other agents had been involved in alleged allergic reactions). Twenty-two patients were considered to have undergone intravascular injections; the remaining 75 were thought to have experienced psychogenic reactions. Symptoms exposed by two patients involved sensory disturbances in contralateral areas distant from the body (limbs) after the administration of lower alveolar nervous block injections. Both events were attributed to intravascular injections with brain distribution of the anesthetic agent since the time of the responses, the absence of other signs (e.g. hyperventilation) and the lack of use of a syringe aspirant for injection. During the skin test procedure, a patient exemplifies some of the problems of the direct test of the challenge by developing irritation at each of the injection sites. It was revealed that he had dermatography (). Figure 3Irritation in each skin injection site (false positive result) 3b Reaction to soft skin strangulation with blunt probe - 'dermatographia'Second group ()Figure 4Second group results The second series of 44 patients were investigated using intra-dermal injection and a direct intraoral challenge. During this period, nine others were sent, but they were not tested. The stories of seven patients so clearly excluded the allergy to local anesthetic agents that treatment was immediately undertaken using adrenaline lymphocaine as a local anesthetic agent. Typically, patients reported regular dental patients and received local anesthesia injections on many occasions earlier. The adverse event was described in various ways, sometimes involving pain, dizziness, fainting or disease. Two patients refused to be tested, one insisting that she was allergic and would seek treatment under general anesthesia 'in another place'. The other patient stated that she suffered from multiple allergies and, on the first visit, said that she should consult her homeopathic (non-medical) doctor. In a second visit, he explained that he had been advised not to submit to tests that "adjust your system." Results of the 44 patients tested Seven patients have been referred because they had informed their dental doctor that they had suffered a previous allergic reaction. None of the stories supported this diagnosis and none of them proved to be allergic to local anesthetic agents. One patient presented evidence that it had been tested and was allergic to 'bisulfites' (their main adverse reactions were foods that contained sulfur preservatives). She had been informed that she was, therefore, allergic to all local anaesthetics. After satisfying the patient about the composition of several anesthesias, the skin tests were performed and it was proved that the patient was not allergic to lignocaine or prilocaine solution. In this case, the dental challenge test was performed with 1.0 ml of 3% Citanest with Octapressin (Astra) without causing a negative response. It was recommended to avoid adrenaline solutions (containing metabisulfite). Three patients had referred because the dental doctor had observed swelling located several hours after treatment, and one patient also developed an eruption. A record indicated that there had been bleeding and inflammation was a hematoma, and allergy tests were negative. The other two may have been allergic to nature, but none of the patients tested positive for local anesthesia. Both patients had received restorative treatment, so they had been exposed to a variety of materials, and one had returned to their doctor for later treatment without local anesthesia, after remission but before the test and had developed localized inflammation again. In these cases, it was recommended that patients be referred to another specialist to identify the provocative material. All remaining patients (33) were referred to by "collapso" after receiving a local anesthesia injection. The details of two patients are interesting: Case 1A patient had experienced her adverse reaction when receiving orthopaedic treatment, after which she was told that the cause was an 'alergia'. Several injections of bupivacaine had been administered to facilitate the manipulation of a painful shoulder. When attempts were made to treat the condition, pain was experienced, so several more injections were given. Shortly after the second injection battery, the patient felt dizzy and could have lost consciousness briefly. The oxygen was administered and recovered slowly. Bupivacaine was included as an additional local anesthesia in the test procedure, without a positive response to any agent. The adverse reaction experienced by this patient was most likely due to systemic toxicity. Case 2The description of another patient's adverse reaction was unusual. It had collapsed shortly after receiving a local dental anesthesia injection, with 'uncontrollable agitation' and respiratory distress. The dentist had witnessed the event and was concerned: an allergic reaction had been suggested as a possible cause. The skin tests were performed and at first the patient was comfortable. While under nursing supervision, about 10 minutes after intra-dermal injections had been completed, the patient began to experience her adverse reaction. This was a typical "panic" attack with tachycardia (the pulse rate increased from 90 to 150), hyperventilation and tetany. There was a slight elevation of systolic blood pressure and oxygen saturation remained constant. The patient was reassured and encouraged to breathe again. Recently, a similar case was reported and the mechanisms related to this reaction have been described: the less severe episodes are quite common. The test procedure was not continued on this occasion. The patient's husband confirmed that the reaction was typical of those experienced earlier. The nature of the response was explained and accepted by the patient and her husband. The skin test was negative, so another visit was advised to undertake the direct dental challenge, but with the patient sedated. This was agreed. On the second visit, the patient announced that, on reflection, it did not agree with the explanation given. Eventually the second challenge test was performed under sedation (intravenous Midazolam) and the patient recovered naturally, without any adverse event up to 50 minutes later when a similar panic attack occurred. It was recommended that the patient need careful support management and that pre-medication or sedation can initially be used to ensure that treatment has been completed. The patient's husband received advice on appropriate responses when panic attacks occurred. The stories of the other 31 patients suggested vasovagal reactions in 25 and probable intravascular administration in 6: none were allergic to any of the anesthetic agents. One of this group referred to a history of collapse associated with 'adjusting': this male patient had a profound fainting during the skin test procedure and seizures were avoided by quickly tilting the chair, so the patient's feet rose. The second dental challenge was administered irregularly, with the patient completely reclined. Follow-up Thirty-two practitioners were contacted to ask about the new management of their patients and 28 responded. Seven patients had not returned to their dental doctor, although two had made appointments, which they did not keep. Six patients had not required a local anesthesia injection. Fourteen patients had been successfully treated using local anesthesia, although three continued to experience problems that the dental surgeons who responded were psychogenic reactions. In one case, it seems that no letters were delivered: the patient received treatment in the hospital under local anesthesia without complication. Recent Wildsmith and colleagues reported on the investigation of 25 patients, who were initially diagnosed as allergic to local anesthetic drugs: most of those patients had received dental treatment. Six of the dental patients suffering from phobia, panic or anxiety were diagnosed and one patient had received intravascular injection (which was affected by the adrenaline content of the cartridge). One of the patients in that series was allergic to metabisulfite. The allergy to latex represented problems with three patients, and the relevance of latex allergy to local dental anesthesia has recently been brought to the attention of the profession. Adverse reactions to local dental anesthesia are common, but most are temporary. Mild systemic reactions are also common due to intravascular injections or rapid absorption if excessive amounts of anesthesia are given. The most significant reactions, which cause concern, are mainly related to some form of "colapso". The results of the research confirm previous reports that the vast majority of systemic reactions to dental injections are caused by: Psychomotor responses (e.g. vasovagal or hyperventilation), and intravascular injections. The most common aspect of dentistry to cause anxiety is an injection, so dental surgeons should be familiar with the variable signs and symptoms of psychological reactions to their treatment. Early management will prevent the development of additional signs of concern (e.g. tetany after hyperventilation; seizures after deep fainting). An aspiration should be performed to prevent intravascular injections. After an adverse reaction has occurred, an explanation is frequently requested. An allergic reaction to local anesthesia should not be suggested. The term 'allergic' is recognized by patients and is easily adopted as the explanation. The experience has shown that the result of the tests reassures some patients, but many remain committed to the original suggestion (and repeat the 'diagnosis' to the next practitioner they consult, which gives rise to another remission and reinforcement of their belief). Local anesthesia is the pillar of pain control during dental treatment, so an adverse reaction should not be misdiagnosed as caused by an allergy, then denying patient access to safe pain control. Despite numerous publications that show that allergy is rare, practitioners still seem to suggest this often as a cause for incessant events. When signs and symptoms develop that are genuinely suggestive of an allergic response, it is more likely that there has been a result of contact with more common allergens (e.g. latex), so again local anesthesia should not be suggested as the probable cause. When there is doubt or where the patient gives a 'final history' (see before), it is important to refer the patient, but to inform them that the tests will be done to confirm the safety of the local anesthesia and, if possible, identify the true cause of the reaction. In very rare cases where a patient is considered to be allergic to one of the anesthesia agents or to one of the other contents of a commercial preparation, an appropriate alternative can be identified. Most adverse reactions to local anesthetic injections can be avoided if the following procedures are adopted: Confidence and care management; (for extremely anxious patients, pre-medication or sedation may be required) Supine positioning of patients (this will prevent most fainting)Aspiration (to prevent intravascular injections)Using preparations that do not contain methylparaben Slow injections (reduce discomfort and improve the location of the solution)Restricting total doses (e.g., not exceeding 300 mg of lignocaine —with or without adrenaline— for a healthy adult male of 7 ml. Conclusions An hundred and forty-one of the adult patients has been investigated because it was suggested that 'allergy' was the cause of adverse reactions that occurred during or immediately after local anesthetic dental injections. In most cases history excluded an allergic reaction. In all cases, a direct skin challenge test (intraérmica) and, in addition, in 44 patients, an intraoral (total typical) challenge test did not achieve an allergic reaction. Adverse reactions to local dental anesthesia injections are common, but most are temporary and may be unnoticed by the dental surgeon. The most common causes of significant reactions are psychogenic (made by anxiety). A lower number of reactions that cause concern are caused by intravascular injections. Some patients suffer from systemic reactions when large amounts of solution are absorbed in circulation. When an adverse event occurs as a result of an injection of local dental anesthesia, the true nature of the problem should be carefully considered. It is important NOT to suggest that there has been an allergic response when clinical events are consistent with well-known common causes of adverse reactions to dental injections. The most adverse reactions are avoidable with attention to the technique. Allergy to ignocaine and other local amide anesthesia used in dentistry is extremely rare. If an acute reaction is strongly suggestive of an allergic response, early remission is required for a thorough investigation. References Sadove M S, Wyant G M, Gittleson L A, Kretchmer H E. Classification and management of reactions to local anesthetic agents. J Am Med Assoc 1952; 148: 17-22.148 Aldrete J A. Sensitivity to Iignocaine. Anaesth Intensity Care 1979; 7: 73–74.7 Brown D T, Beamish D, Wildsmith J A W. Allergy reaction to a local amide anesthesia. Br J Anaesth 1982; 54: 435-437.54 G, Schatz M, Patterson R, Rosenberg M, Yamamoto F, Hamburger R N. Local anesthesia administration to patients with prior adverse reaction history. J Allergy Clin Immunol 1978; 61: 339-345.61 From Shazo R D, Nelson H S. A patient approach with a history of local anesthetic hypersensitivity: Experience with 90 patients. J Allergy Clin Immunol 1979; 63: 387-394.63 Barer M R, McAllen M K. Hypersensitivity to local anesthesia: a direct challenge test with lignocaine for definitive diagnosis. Br Med J 1982; 284: 1229-1230.284 Noble D S, Pierce G F M. Alergia a Iignocaine. A historic case. Lancet 1961; 281: 1436.281 Bateman P B. Multiple allergies to local anesthesia including prilocaine. J Med Aust 1974; 2: 449–452.2 Johnson W T, Stigter T. Procaine hypersensitivity, tetracaine, mepivacaine and methylparaben: report of a case. J Am Dent Assoc 1983; 106: 53–56.106 Luebke N H, Walker J A. Discussion of sensitivity to preservatives in anesthesia. J Am Dent Assoc 1978; 97: 656-657.97 Schwartz H J, Sher T H. Sensitivity bisulphite manifesting as an allergy to local dental anesthesia. J Allergy Clin Immunol 1985; 75: 525-527.75 Wildsmith J A W, Mason A, McKinnon R P, Rae S M. Alleged allergy to local anaesthetic drugs. Br Dent J 1998; 184: 507-510.184 Aldrete J A, O'Higgins J W. Evaluation of patients with a history of allergy to local anesthetic drugs. Southern Med J 1971; 64: 1118–1121.64 Ezsias A. Lignocaine and allergy anesthesia. Br Dent J 1998; 185: 428.185 Spiers R L, Barsby M J. Hyperventilation in the dental chair. Dent Update 1995; 22: 95–98.22 Campo E A, Davies M, Longman L P, White J F. Latex allergy. Br Dent J 1997; 182: 410.182 Rood J P. LA – Safe work dose. National Dental BDA Conference. April 1999. Fiset L, Milgrom P, Weinstein P, Getz T, Glassman P. Psychophysiological responses to dental injections. J Am Dent Assoc 1985; 111: 578–583.111 Meechan J G, Rood J P. Aspiration in local dental anesthesia. Br Den J 1992; 172: 40,172 General Dental Council. Maintain rules. May 1999. Author's information Affiliates Professor, Consultant in Oral and Maxillofacial Surgery, GKT Dental Institute, King's College Hospital, Caldecot Road, London, SE5 9 RWJ P Rood You can also search this author in Additional information Reference document Documents and permissions About this article Cite this article Rood, J. Adverse reaction to injection of local dental anesthesia — 'allergy' is not the cause. Br Dent J 189, 380–384 (2000). https://doi.org/10.1038/sj.bdj.4800776189, Received: 27 October 1999Accepted: 12 April 2000 Published: 14 October 2000Entry date: 14 October 2000DOI: Explore contentGeneral information Publish with usSearch Quick links British Dental Journal ISSN 1476-5373 (online) nature.com sitemap Discover contentPublication policiesAuthor & Research services Libraries and institutions Advertising and partnerships Professional development Regional websites Legal © 2021 Springer Nature Limited
What you need to know about dental anesthesia Is it programmed for a dental procedure and has questions about anesthesia? Around people have anxiety and pain concerns with dental procedures. Anxiety can delay treatment and that can make the problem worse. Anesthetics have been out there for over 175 years! In fact, the first procedure registered with anesthesia was performed in the use of ether. Since then we have made a lot of progress, and anesthesia is an important tool to help patients feel comfortable during dental procedures. With many options available, anesthesia can be confusing. We decompose it so you feel safer before your next dental appointment. Anesthesia means lack or loss of sensation. This can be with or without consciousness. Today there are many options available for dental anesthesia. Medicines can be used alone or combined for a better effect. It is individualized for a safe and successful procedure. The type of anesthesia used also depends on the person's age, state of health, duration of the procedure and any negative reaction to anesthesia in the past. Anesthetics work in different ways depending on what is used. Anesthesia can be short-acting when it is applied directly to an area or work for longer when more involved surgery is required. The success of dental anesthesia depends on:Other things that may affect dental anesthesia include the time of the procedure. It also shows that inflammation may have a negative impact on the success of anesthesia. In addition, for local anesthesia, the teeth at the bottom of the jaw (mandibular) of the mouth are more difficult to anesthesia than the teeth of the upper jaw (maximum). There are three main types of anesthesia: , sedation and . Each has specific uses. These can also be combined with other medicines. Local anesthesia is used for simpler procedures such as cavity filling, which requires a shorter time to complete and is usually less complicated. You will be aware and able to communicate when you have a local anesthesia. The area will be numb, so you won't feel pain. Most local anesthesias have a quick effect (in 10 minutes) and last 30 to 60 minutes. Sometimes anesthesia is added to an effect like epinefrine to prevent anesthetic effect from being extended to other areas of the body. Local anesthetics are available at the counter and as a recipe in gel, ointment, cream, spray, patch, liquid and injectable forms. They can be used topically (applied directly to the affected area for numbing) or injected into the area to be treated. Sometimes light sedation is added to local anesthesia to help relax a person. Examples of local anesthesiaEducation has several levels and is used to relax a person who may have anxiety, help with pain or keep them quiet for the procedure. It can also cause procedural amnesia. You could be totally and able to respond to commands, semi-conscious or barely conscious. The building is categorized as mild, moderate or deep. Deep sedation can also be called monitored anesthesia care or . In deep sedation, you are generally not aware of your environment and can only respond to repeated or painful stimulation. The medication may be given orally (table or liquid), inhaled, intramuscularly (IM) or intravenous (IV). There are more risks with sedation IV. Your heart rate, blood pressure, and breathing should be carefully monitored in moderate or deep sedation. Medicines used for sedationThe general anesthesia is used for longer procedures, or if you have a lot of anxiety that might interfere with your treatment. You'll be completely unconscious, painless, your muscles will be relaxed, and you'll have amnesia of the procedure. The medication is given through a facial mask or IV. The level of anesthesia depends on the procedure and the individual patient. There are different risks with general anesthesia. The side effects of dental anesthesia depend on the type of anesthesia used. General anesthesia has more risks than local anesthesia or sedation. Reactions also vary according to individual factors. Some side effects reported with sedation medications and general anesthesia include: such as epinefrine added to anesthetics may also cause heart and blood pressure problems. These are some reported side effects of anesthesia. Ask your dental care team about your specific medication and any concerns you may have about the medication. There are conditions and situations in which you and your doctor or dentist will discuss whether dental anesthesia is the best choice for you. The consent for treatment is an important part of the pre-treatment discussion. Ask questions about the risks and safety precautions that will be taken to ensure a positive outcome. Pregnancy If you are pregnant, your dentist or surgeon will discuss the risks against the benefits of anesthesia for you and your baby. Special NeedsChildren and people with special needs require careful evaluation of the type and level of anesthetics they need. Children may need dose settings to avoid adverse reactions or overdose. The Food and Drug Administration (FDA) issued a numbing agent approach commonly used for tooth pain. These products are not safe for use in children under 2 years of age. Do not use these medications without arguing with a health professional. Children and adults with special needs may have other medical complications that increase the risks with anesthesia. For example, children with cerebral palsy had the largest number of adverse reactions related to the airway to general anesthesia. Older adults Older adults with certain health problems may need dose settings and careful follow-up during and after surgery to ensure their safety. Some people may experience delirium or confusion and memory problems after surgery. Problems of liver, kidney, lung, or heart People with liver, kidney, lung, or heart problems may need to adjust the dose because the medication may take longer to leave the body and have a more powerful effect. Certain neurological conditions If there is a history of stroke, Alzheimer's disease, Parkinson's disease, thyroid disease, or mental illness, there may be a higher risk with general anesthesia. Other conditions Make sure your dental team knows if you have a , , infections or sores open in your mouth, allergies, severe nausea and vomiting with anesthetics, or are taking any medication that can make you sleep like . People at risk of dental anesthesiaThe belts are also higher for those with: The risks are also greater for those with: Most people do not experience adverse reactions with local anesthesia. There are greater risks with sedation and general anesthesia, especially in older adults and people with other health complications. There is also a growing risk with history of hemorrhagic disorders or medications that increase the risk of bleeding as aspirin. If you are taking pain medications such as opioids or anxiety medications such as , tell your dentist or surgeon so you can adjust your anesthesia accordingly. Anesthesia Risks Anesthesia risks include: Anesthesia-related anxiety is common but may complicate treatment. It is important to discuss all your concerns about the procedure and your expectations with your dental care team before. Ask questions about the medications that will be used and what you can expect during and after treatment. Share your medical history, including any allergies and other medications you are taking. Make sure this includes over-the-counter medicines, prescriptions and supplements. Ask about the special instructions you need to follow before and after the procedure. This includes food and drink before and after treatment. Ask if you need to arrange transportation after the procedure and any other information you need to know. Your dental provider will give you instructions to follow before and after the procedure. They will also provide a way for you to contact them in case you have any complication or question. Last medical review on December 13, 2019Read this following
Adverse reaction to dental local anaesthetic injection — 'allergy' is not the cause | British Dental Journal
Figure 3 from Anaesthesia: Adverse reaction to dental local anaesthetic injection — 'allergy' is not the cause | Semantic Scholar
Allergic reactions to dental materials, drugs require an alert response from practitioner | Registered Dental Hygienist (RDH) Magazine
Local and Regional Anesthesia in Dental and Oral Surgery | SpringerLink
Hypersensitivity to Local Anesthetics: A Case Report
Allergic Reaction Associated with the use of Eugenol Containing Dental Cement in a Young Child
Local Anesthesia: Uses, Types, Process, Risks, and Pregnancy Safety
Adverse reactions to local anesthetics | Registered Dental Hygienist (RDH) Magazine
Local Anaesthetic Allergy & Testing
Figure 1 from Anaesthesia: Adverse reaction to dental local anaesthetic injection — 'allergy' is not the cause | Semantic Scholar
Superficial skin necrosis and neurological complications following administration of local anaesthetic: a case report - Pattni - 2013 - Australian Dental Journal - Wiley Online Library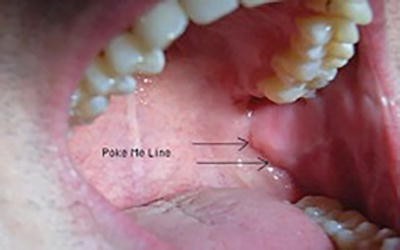
Local and Regional Anesthesia in Dental and Oral Surgery | SpringerLink
Techniques for effective local anaesthetic administration for the paediatric patient | British Dental Journal
allergies Archives - Directions in Dentistry
Reversing Local Anesthesia | Inside Dentistry
Intraligamentary anesthesia – a brief review of an underestimated anesthetic technique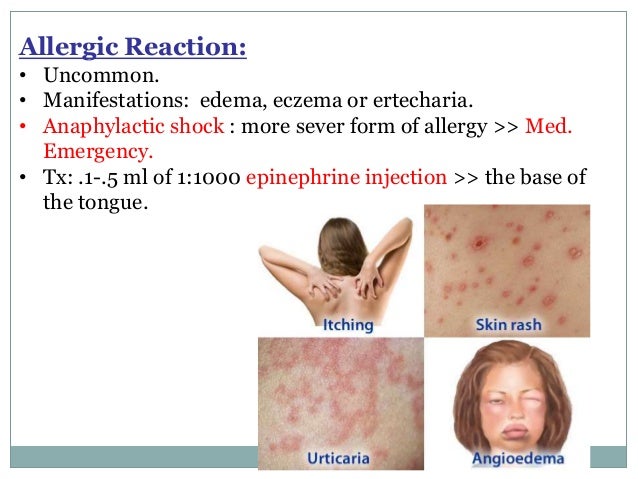
Local Anesthesia for pediatric dentistry
Techniques for effective local anaesthetic administration for the paediatric patient | British Dental Journal
Local Anesthesia: Uses, Types, Process, Risks, and Pregnancy Safety
Local anesthesia in dental practice - Docsity
Overview of Local Anesthesia Techniques | IntechOpen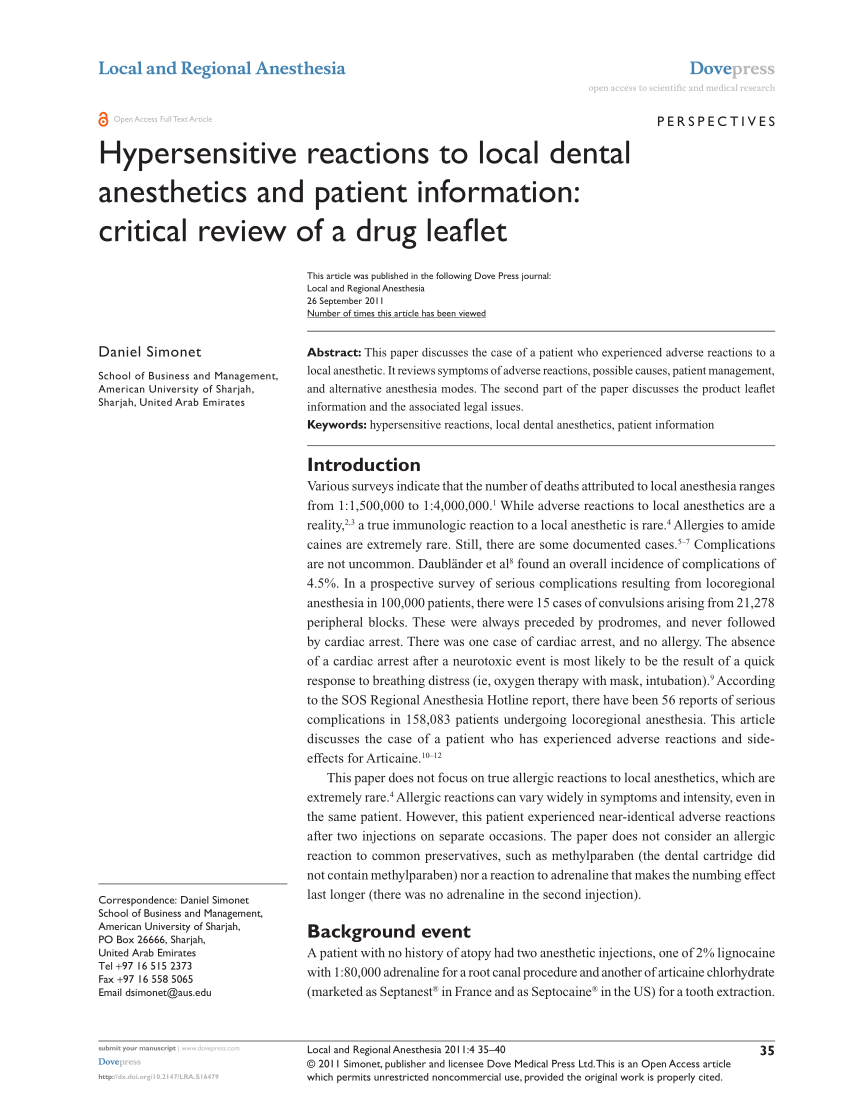
PDF) Hypersensitive reactions to local dental anesthetics and patient information: Critical review of a drug leafet
MAC Anesthesia (Monitored Anesthesia Care)
Adverse drug reactions to local anesthesia
Anesthesia - Wikipedia
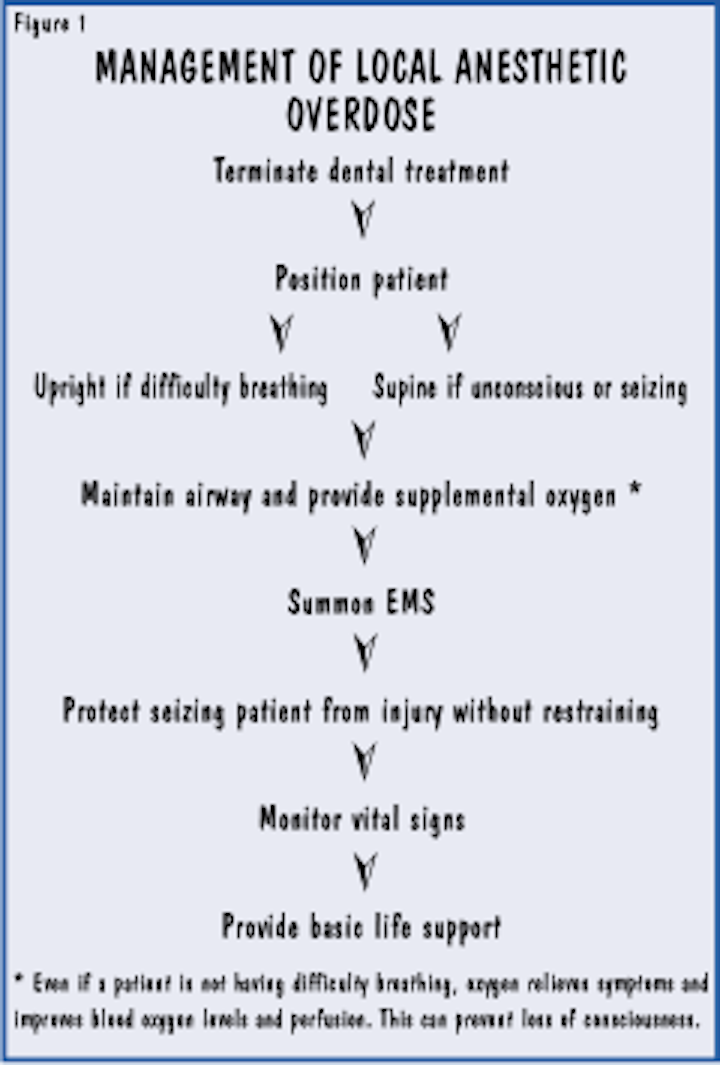
Complications of Local Anesthesia | Adverse Effects of Local Anesthesia
Infiltrative Anesthesia in Office Practice - American Family Physician
Local Anaesthetic Allergy & Testing
Allergic reactions to anesthesia - Wikipedia
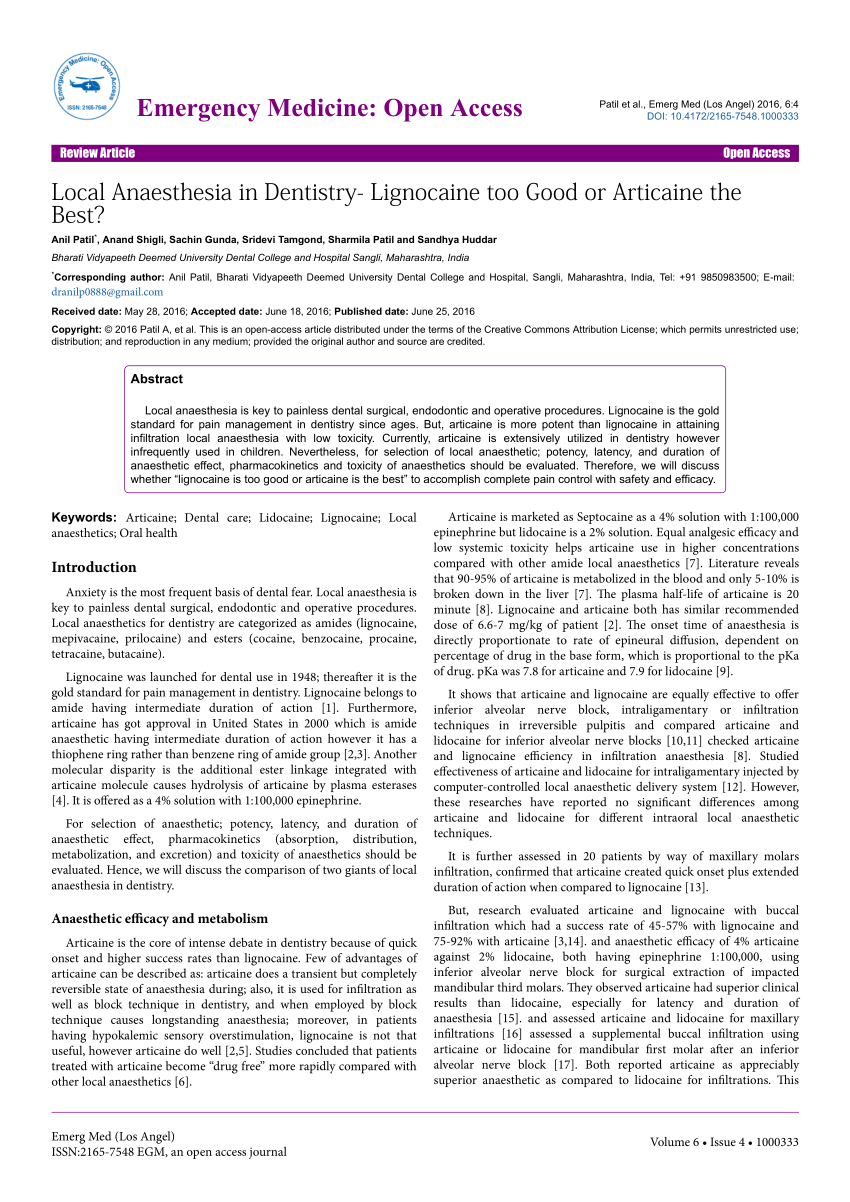
PDF) Local Anaesthesia in Dentistry- Lignocaine too Good or Articaine the Best?
Adverse reaction to dental local anaesthetic injection — 'allergy' is not the cause
PDF) Dental anesthesia for patients with allergic reactions to lidocaine: two case reports
Local anesthesia: Uses, types, and risks
Dental anesthesia for patients with allergic reactions to lidocaine: two case reports. - Abstract - Europe PMC
Safety of buccal infiltration local anaesthesia for dental procedures - Dougall - 2019 - Haemophilia - Wiley Online Library
Dental Managment Of Allergy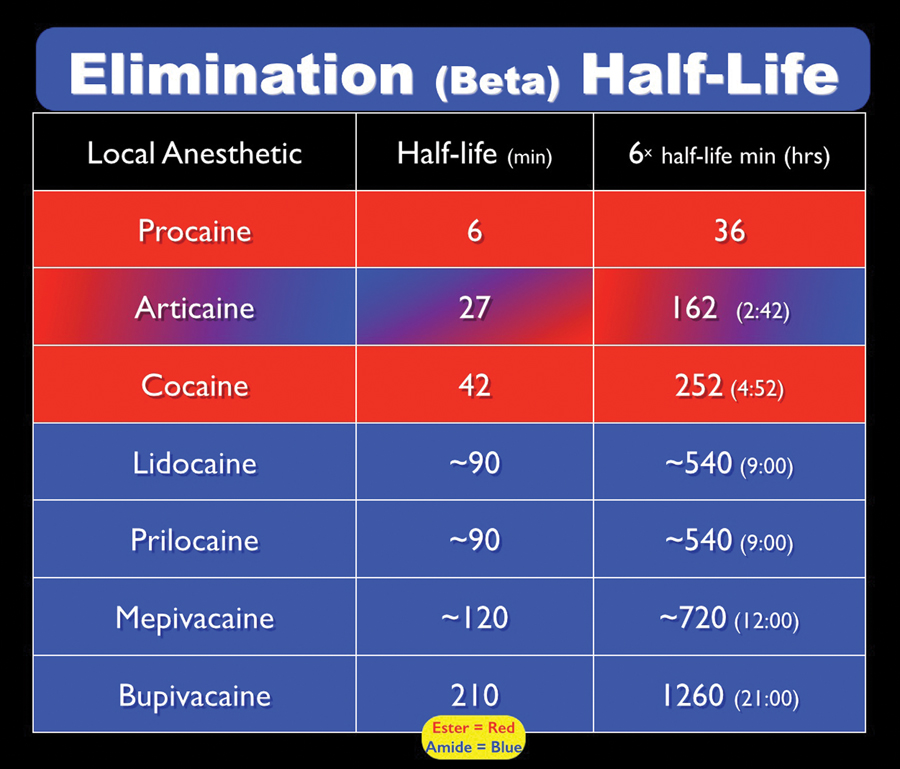
ARTICAINE 30 Years Later - Oral Health Group
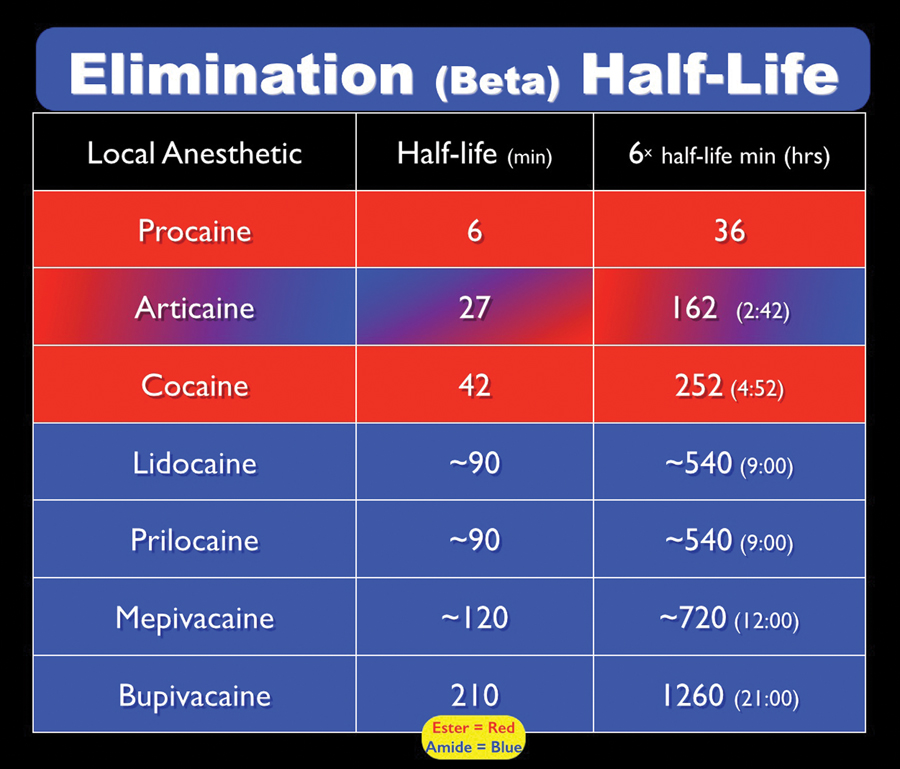
PDF) Local Anesthetics: Pharmacology and Toxicity
Superficial skin necrosis and neurological complications following administration of local anaesthetic: a case report - Pattni - 2013 - Australian Dental Journal - Wiley Online Library
How Long Does Dental Anesthesia Last? FAQs | Legacy Dental | Legacy Dental
 Adverse reactions to local anesthetics | Registered Dental Hygienist (RDH) Magazine
Adverse reactions to local anesthetics | Registered Dental Hygienist (RDH) Magazine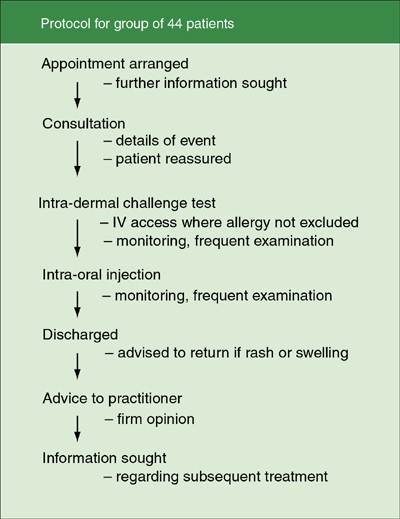























Posting Komentar untuk "adverse reaction to dental anaesthetic"